The Science of Ketamine: How It Helps Treatment-Resistant Depression
Struggling with depression that hasn’t improved with traditional medications? Learn how ketamine treatment at Black Psychiatry in Utah works on the brain to rapidly relieve treatment-resistant depression and enhance neuro-plasticity.
Why Traditional Psychiatric Treatments May Fall Short
Traditional medications don’t always address the root causes of depression and anxiety. Discover how functional psychiatry at Black Psychiatry in Utah looks deeper-hormones, inflammation, gut health, sleep-to deliver lasting mental wellness.
Real Transformation: Patient Stories from Ketamine Treatment
At Black Psychiatry, we’ve witnessed remarkable transformations through ketamine treatment. For many patients, it’s not just another medication-it’s the moment they finally begin to feel again, to hope again, and to see light where there was once only darkness.
Functional Medicine in Psychiatry: Looking Beyond Symptoms
At Black Psychiatry in Utah, we go beyond symptom relief. Discover how functional medicine in psychiatry identifies root causes-hormones, nutrition, sleep, and inflammation-to create lasting mental health solutions.
How Nutritional Psychiatry Supports Better Mental Health Outcomes
Discover how nutrition impacts depression, anxiety, and brain health. Black Psychiatry in Utah integrates nutritional psychiatry with advanced care to improve mental wellness and long-term outcomes.
Ketamine Treatment: What to Expect from a Protocol at Black Psychiatry
Curious about ketamine treatment in Utah? At Black Psychiatry, we provide safe, medically supervised ketamine protocols to help with depression, PTSD, and anxiety. Learn what to expect before, during, and after treatment.
Lifestyle, Sleep, and Movement: The Unsung Pillars of Mental Health
Discover how better sleep, daily movement, and lifestyle changes can transform mental health. We in Utah integrate holistic strategies with advanced psychiatric care for lasting wellness.
Why Ketamine + Psychotherapy Is a Powerful Combination
Discover how combining ketamine therapy with psychotherapy in Utah enhances neuroplasticity, rewires the brain, and supports lasting healing. Learn why integration therapy is key at Black Psychiatry.
ketamine-assisted psychotherapy Utah
ketamine therapy with counseling Utah
ketamine psychotherapy integration Utah
ketamine and therapy for depression Utah
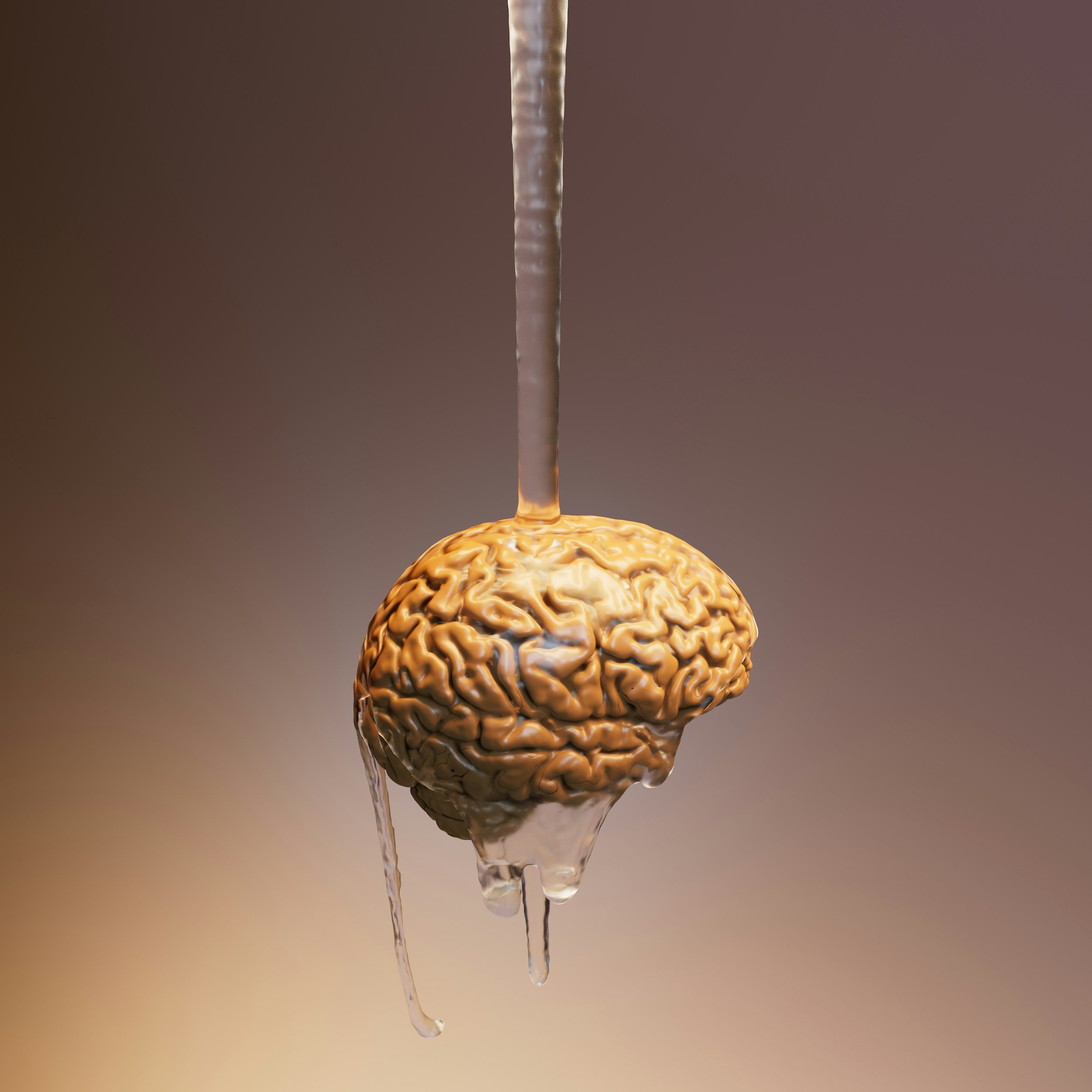
neuroplasticity and ketamine
integration therapy after ketamine
psychotherapy during ketamine treatment
emotional healing with ketamine
ketamine therapy Utah provider
best ketamine-assisted psychotherapy in Utah
what to expect from ketamine and therapy sessions
combining ketamine with talk therapy Utah
is ketamine therapy more effective with psychotherapy?
how ketamine therapy rewires the brain Utah
Ketamine Therapy Safety: What You Need to Know Before Starting Treatment
Looking for safe ketamine treatment in Utah? At Black Psychiatry, we provide thorough medical screening, expert supervision, and personalized care to ensure effective, life-changing results for depression, PTSD, and anxiety.
Concierge Psychiatry: A Smarter, More Personal Approach to Mental Health
Mental health treatment shouldn't feel like you're being rushed through a system. At Black Psychiatry, we believe that healing starts with being heard. That’s why we’ve chosen a different path-one that prioritizes time, attention, and a deep partnership with every patient.
This is the heart of Concierge Psychiatry.
How Ketamine Works on the Brain: The Science Behind Its Transformative Power
In recent years, ketamine has captured the attention of clinicians, researchers, and patients alike for its rapid and often life-saving effects in treating depression, anxiety, and emotional pain. At Black Psychiatry, we’re not only interested in that ketamine works—we’re deeply invested in understanding how it works. The science is fascinating, and more importantly, it’s hopeful.
Ketamine in Utah. Ketamine Treatment in Utah. Ketamine SLC
Let’s break it down in plain terms.
Ketamine Treatment: Fast, Effective Relief for Depression & Emotional Pain
Learn how ketamine therapy—led by Dr. Black—offers rapid relief for treatment-resistant depression, PTSD, anxiety, and suicidal thoughts, with evidence-based benefits and safety considerations. Ketamine in Utah. Best Ketamine Treatment in Utah
Holistic Anxiety Relief: How to Calm Your Nervous System Naturally at Home
Discover natural and easy ways to reduce anxiety at home. Learn how to activate your vagus nerve, use ice packs, and practice holistic methods that support your mental health. Mental health and Ketamine Utah
How Your Gut Creates Serotonin — And Why It’s a Big Deal for Your Mental Health
When we think about mental health, we often focus on the brain. But what if I told you one of the biggest influencers of your mood, anxiety levels, and even sleep patterns is actually in your gut?
KetamineTreatment: A New Hope in Mental Health Care
Best Ketamine in Utah! Over the past decade, mental health treatment has experienced a quiet but powerful revolution. Having a nutritional psychiatry focus, I’ve seen firsthand how conventional approaches—therapy, SSRIs, mood stabilizers—can be life-changing for many, but not for everyone. Some patients remain stuck in a fog of depression, a multitude of side effects and despite trying numerous medications, therapists, and every self-help book under the sun.